- Home
- Benefits of Massage
- Scar Tissue Massage
As an affiliate with Bookshop, Amazon, and other programs, I may earn revenue from qualifying purchases through affiliate links. This does not affect the price you pay. Privacy Policy / Disclosures. This site is for educational purposes only.
Search this site:
How Can Massage Help Scar Tissue and the Healing Process?
When discussing massage and scar tissue, we need to look at two types: massage of external scar tissue from healed wounds and massage of internal scar tissue and adhesions that form when you have a soft-tissue injury.
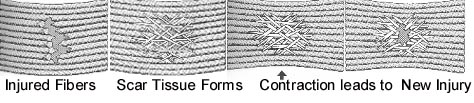
The formation of scar tissue is an essential part of the healing process. However, this tissue is weaker, less elastic, more likely to be re-injured, and more sensitive to pain than healthy tissue. Massage can improve the quality of scar tissue.

Can Massage Help Scar Tissue from External Wounds?
Scar tissue massage after surgery or other skin injury can stop excess tissue from building up and help make scars less noticeable.
Massage softens and flattens scars and reduces the adhesions between the layers of tissue. Benefits of massaging a scar:
- Reduce itchiness, tightness, or over-sensitivity.
- Improve the flexibility, mobility, and softness of scar tissue.
- Influence collagen to form scar tissue more evenly.
- Prevent the scar from becoming hard and inflexible, which can inhibit movement, especially if a scar crosses a joint.
When to start massage? Start massaging a scar when the wound is completely healed. If in doubt, ask your healthcare provider.
You can massage old scars, but the effect will typically be less and will take longer.
How to Massage Scar Tissue
Use the pads of two fingers or your thumb to massage the scar and surrounding tissue, following these guidelines:
- Do not let your fingers slide on the skin. You want to move the scar tissue.
- Massage in all directions: side to side, up and down, and circular motions.
- Begin with light pressure and progress to deeper and firmer pressure. Use as much pressure as you can without significant discomfort.
- Massage your scar regularly, generally two or three times a day for five minutes at a time. However, if you feel pain or the area becomes oversensitive, stop massage for the day and start again the next day.
- Continue massage for at least three to six months or until you see and feel a significant difference.
Note: You can use a small amount of moisturizer, if needed, but remember you don't want your fingers sliding over the skin.
Video: How to Do Scar Massage

You can also combine massage with essential oils for external scars.
Scar tissue massage tools are available.
How Can Massage Help Scar Tissue Internally?
An adhesion is an internal band of scar tissue that binds together tissue fibers, preventing them from moving properly. When adhesions develop on muscles, fascia, or other connective tissue, they can limit the movement ability of a muscle or joint.
The Healing Process and Massage
When you have a soft-tissue (muscle, tendon, ligament, etc.) injury, it heals in three stages called the inflammatory response.
Acute phase (lasts 2 to 4 days): Initially, acute inflammation, redness, swelling, heat, and pain occur. The fluids from torn blood and lymph vessels coagulate to seal off the injured area, while uninjured vessels bring in extra fluids and chemicals that create a gel-like substance around the injured tissue. This gel contains binding factors that help hold together the injured tissues.
During the acute phase, white blood cells called macrophages come in to eat the dead tissue and bacteria that might cause infection. The macrophages also let the body know how many repair cells called fibroblasts to send in. If infection or prolonged inflammation occurs, the macrophages request too many fibroblasts, contributing to the formation of excess scar tissue.
During the acute phase, gentle massage to surrounding areas helps reduce swelling by assisting fluid movement, but direct massage to the injury can cause damage.
Repair or rebuilding phase (lasts 3 to 4 weeks): As inflammation decreases, fibroblasts begin to repair the injured tissue by producing collagen and lubricating fluids. The collagen fibers line up within the fluid and bond, forming scar tissue over the injury. During this phase, gentle movement, range of motion, and gentle massage can help the collagen fibers move, line up, and bond normally.
Some sources recommend starting to massage scar tissue 8 to 16 days after the initial injury for the best results, though your individual situation may vary. Newer scars are more malleable.
Remodeling phase (lasts 6 to 12 months): The body works to return the tissues as closely as possible to their original condition. The collagen making up the scar tissue is constantly being replaced. How well the fibers align in the final scar tissue depends on a number of factors. One of the most important is the pulling tension (tensile force) the scar tissue experiences during remodeling. Now is the time that scar tissue massage is particularly helpful because it creates tension.
Cross-Fiber Friction
Although there are various scar massage techniques, a common one is cross-fiber friction, which is often used as part of injury massage. Effectively using this technique requires precision. The massage therapist must locate the adhesion and then apply pressure to move across the fibers without sliding over the skin.
Cross-fiber friction can be uncomfortable, but the massage therapist should always do the technique within your pain tolerance. The discomfort gradually decreases over a number of sessions as excess scar tissue goes away and the remaining scar tissue becomes stronger.
The following video demonstrates cross-fiber friction massage for tennis elbow:
Scar tissue image adapted from an early edition of A Massage Therapist's Guide to Pathology by Ruth Werner.




